Research reveals clues to why immune cells seem to cause brain damage
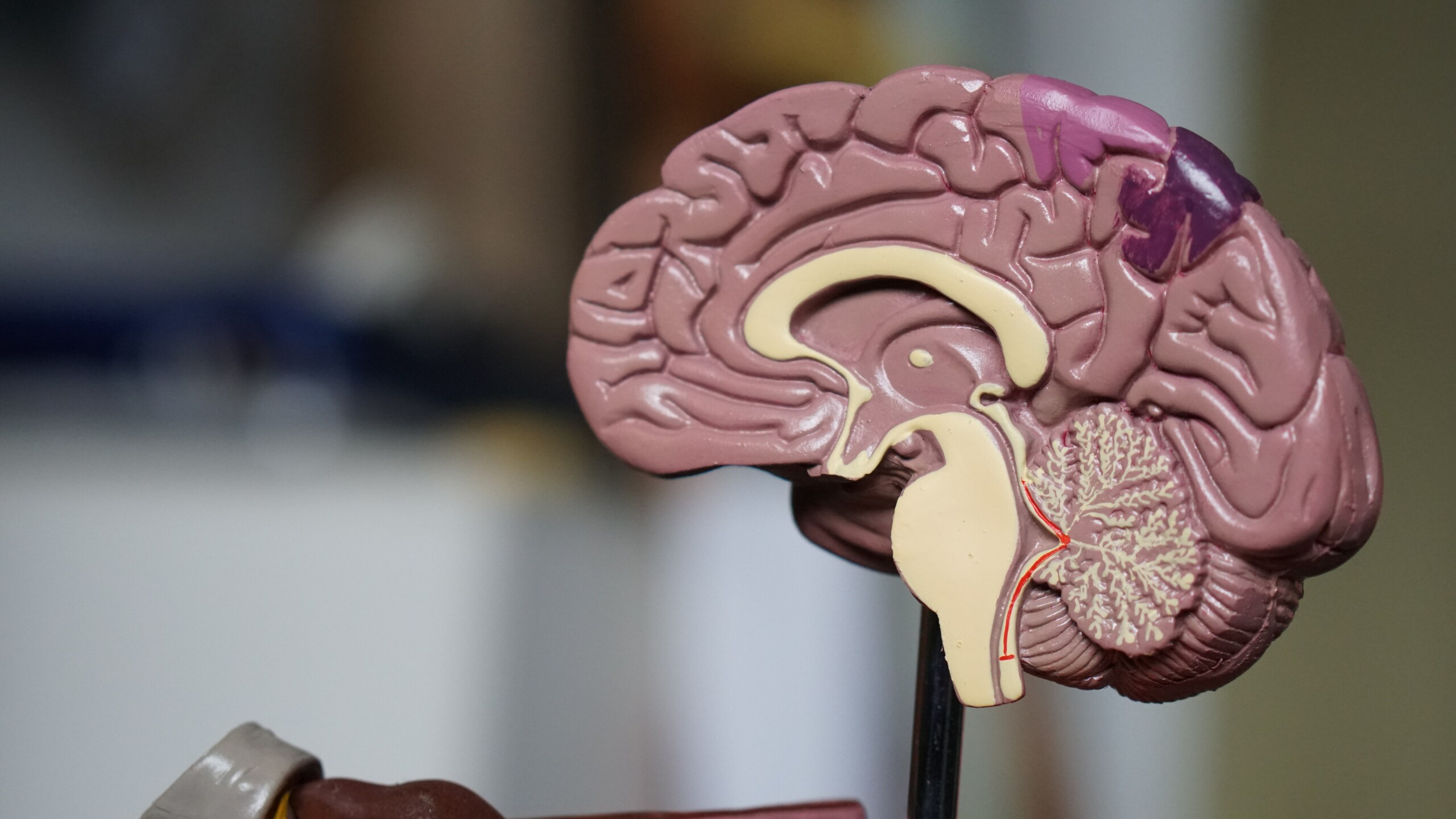
Photo by Robina Weermeijer
In the human central nervous system, there are tiny cells that — for most people, most of the time — provide important immune protection to the brain and spinal cord. Occasionally these microglia cells run terribly awry, leading to neurodegenerative diseases like multiple sclerosis and Alzheimer’s.
But in a recent study, University of Alberta researchers have found new information about how these immune cells change and respond to injury — a discovery that could help in the search for ways to protect the human brain when these cells go bad.
“We know that under certain conditions the microglia are profoundly important for regeneration — and we also know that under other conditions they may have seemingly neurotoxic properties,” says Jason Plemel, assistant professor of neurology in the Faculty of Medicine & Dentistry and Canada Research Chair in Glial Neuroimmunology.
Plemel and his team are searching for ways to direct the central nervous system’s immune response to minimize further damage.
“Our lab is studying the yin and yang of microglia — we’re really trying to understand if and how the microglia become neurotoxic.”
Understanding immune cell behaviour
In the study, Plemel’s laboratory was trying to find out how microglia behave when demyelination — that is, damage to the myelin, or insulating material that coats most neurons — is chemically induced in animal models. Multiple sclerosis is a demyelinating disease.
Previous research has shown that microglia play a large role in demyelination. In fact, in this type of model, from the earliest stages, if you get rid of microglia throughout, no demyelination occurs.
But that’s only part of the story, Plemel explains, because the role of microglia is complex.
“We saw that when we remove microglia in later stages, there is no change in demyelination. And microglia are almost exclusively responding to the injury and behave in the way we would think immune cells respond. They consume debris and lytic cells, cells that died in an inflammatory way, in this diseased model,” says Plemel.
In the study, the researchers also compared the microglia in the MS injury model with those that had been described in previous research on an Alzheimer’s disease model and found that “they look very similar,” according to Plemel.
“This tells us that the microglia immune cells present in MS white-matter injury have similar characteristic states and functions to the ones in Alzheimer’s disease,” he notes.
Pointing the way toward treatments
Plemel says it has been generally accepted that the immune cells can be neurotoxic but he doesn’t think that has been fully proven. By continuing in-depth study of the microglia, he hopes to be able to identify toxic attributes or properties — and “maybe make neurotoxic microglia less injurious.”
“What it means for people with MS is that if their brains’ immune cells were to become toxic under certain conditions, then this research could open up a new way to protect their brains against damage.”
The study, “Single-cell microglial transcriptomics during demyelination defines a microglial state required for lytic carcass clearance,” was published in Molecular Neurodegeneration.
Jason Plemel is also a member of the Neuroscience and Mental Health Institute and the Multiple Sclerosis Centre at the U of A.
